Medication Support
Scope of this chapter
Many of the people we support need to take medication. This includes both prescribed and unprescribed medication.
It is paramount that all medication activities are carried out safely, but opportunities to promote independence, choice and control must also be maximised.
This chapter provides guidance about good general practice when supporting people to take their medication.
The CQC website contains detailed guidance for each type of care setting and information on the requirements for specific medicines, conditions or circumstances:
CQC: Medicines information for adult social care services
The registered person should use the CQC guidance to inform service policy and/or procedure regarding ordering, transporting, storage, preparation, administration and disposal of different medicines in the service.
The CQC also has a dedicated email for medication advice and support: medicines.enquiries@cqc.org.uk
Relevant Regulations
Related Chapters and Guidance
- Choice and Control
- Consent
- Information and Guidance for Specific Safeguarding issues
- Mental Capacity
- Promoting Independence and Strengths
- Risk Assessment (person-centred)
- Safe Care and Treatment
- CQC: Medicines information for adult social care services
- CQC: Covert administration of medicines
- CQC: Medicines administration records in adult social care
Amendment
In April 2023, this chapter was updated. Links to individual CQC guidance documents were deleted and replaced with a link to the relevant CQC webpage. In Section 1, further guidance about the use of medication as restraint was also added.
The following are some of the important principles that apply when providing medication support:
- Medication procedures must always reflect current regulations around ordering, transporting, storing, administering and disposing of medicines;
- Nobody must carry out medication tasks until they are fully competent, skilled and knowledgeable to do so;
- Prescription medicines must always be given in line with the instructions of the prescriber;
- Full and proper records of medicine administration must always be kept;
- Consent must always be sought before administering medication;
- Medication must be administered in ways that uphold dignity;
- Opportunities to promote independence, choice and control should always be maximised;
- Covert administration of medication can only be used if a best interest decision has been made by a medical professional or a court under the Mental Capacity Act 2005;
- Medication must never be used as a form of punishment and may only be used as a form of restraint where a best interests decision has been made as such under the Mental Capacity Act 2005. (see 1.1 below).
Restraint is defined under the Mental Capacity Act as:
- Any act that uses, or threatens to use, force to carry out another function to which the person resists; or
- Any act that restricts the person's freedom of movement, whether or not they resist.
Under section 6 of the Act a best interest decision cannot authorise the use of restraint, unless:
- The decision maker believes that it is necessary to restrain the person in order to prevent them from being harmed; and
- There is evidence that restraint is a proportionate response to the likelihood and seriousness of harm.
Supporting someone with medication is an opportunity to promote independence, choice and control. The importance of these principles and values are explained in separate chapters of this Handbook, which you should refer to as required:
Self-medication happens when a person can manage their medication with minimal hands-on support. This includes visiting the GP, collecting or ordering prescriptions, storing medication and taking it as instructed.
Minimal hands-on support includes things like:
- Occasional reminders or prompts (verbal or through technology);
- Opening bottles or popping out pills if the person has reduced dexterity;
- Support to read or understand the patient information leaflet;
- Support to understand whether over the counter medication is compatible with prescribed medication.
If we recognise someone may be able to self-medicate, we should take steps to support them to do so. This could involve adding goals to an individual care or support plan or supporting them to access technology.
Consent must always be sought before administering medication. A person has the right to refuse to take their medication at any time.
Where possible, consent should be sought prior to preparing medication. This helps prevent unnecessary waste of medication should the person subsequently decide not to take it.
For guidance on consent see: Consent
If a person refuses to take their medication, you should explain the potential negative consequences and establish whether they understand them. If they do understand they have capacity and deciding not to take the medication is their choice, even if the decision appears to be unwise.
Where there are concerns that the person may not understand the reasons why the medication should be taken, a formal assessment of their capacity to make decisions about taking or refusing the medication should be carried out by an appropriate professional. This would normally be their GP.
For guidance on mental capacity see: Mental Capacity.
Medical advice should be sought whenever medication is refused to ensure their safety is not compromised by the decision they have made. Depending on the likelihood and severity of potential consequences, this could be telephoning the GP or Pharmacist, or it could be calling 101 or 999 for more urgent medical advice. We have a duty of care, so this advice can be sought without the person’s consent.
In all cases you should also try to find out why someone does not want to take their medication. There could be many reasons for this, some of which can be easily rectified.
For example:
- It may taste horrible;
- It may be difficult to swallow;
- It may have negative side effects they want to avoid;
- They may not believe the medication is helping them;
- They may not want you to give it to them;
- They are tired and don’t feel like taking it at that time.
Potential solutions to rectify the above could be:
- Providing a flavoured drink with the tablet;
- Speaking to the GP about more palatable options;
- Looking at the patient information leaflet to explain what the medication does;
- Asking a medical professional to explain what the medication does;
- Asking a colleague to administer the medication;
- If the medication is not time specific, trying to administer it later.
Note: Under no circumstances must anyone administer medication covertly, unless the person lacks capacity to refuse consent and crushing, hiding or disguising their medication has already been determined by a medical professional or a court to be in their best interests. Guidance about covert medication is provided in section 7. below.
A record must be made of the refused medication, why it was refused, any views on the person’s capacity to make this decision and what action was taken to ensure safety was not compromised. Any advice given by a medical professional should be clearly recorded. Full guidance on recording can be found below: Recording administration of medication.
The person’s individual care or support plan and/or medication risk assessment must be updated where necessary. Any changes must be communicated to anyone that administers medication.
Needs, preferences, and risks must be established before the service begins.
A formal review of needs, preferences and risks should take place annually, and whenever there are signs that needs, preferences or risks have changed. For example, a medication is stopped, started or dosage is changed.
|
Personal details |
|
|
Health professionals |
|
|
Known allergies |
|
|
Prescribed medications (regular) |
|
|
Prescribed medication (PRN) |
|
|
Over the counter medication |
Services should only support with the administration of unprescribed medicines when a GP has given approval to this. |
|
Known issues with medicines |
For example:
|
|
What can the person do independently and what do they need support with? |
People often need support with only one or two elements of a task. Break the task down and maximise opportunities for independence. |
|
Preferences and cultural needs |
For example:
|
All needs and preferences must be recorded in the individual care or support plan and communicated to staff.
Before preparing medication, anyone that will be involved in handling medicines must wash their hands and put on any PPE that has been deemed necessary for the task.
To wash hands effectively, see below.
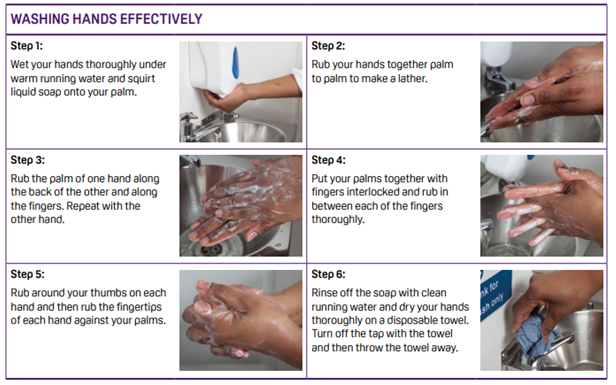
Source: Food Standards Agency
If you think another member of staff has not washed their hands, emphasise how important it is to wash their hands when working with medication. If they do not wash them straight away tell a manager or the registered person.
Disposable gloves
If the service uses disposable gloves for medication, this is not an alternative to effective handwashing. Hands should be washed before using gloves and afterwards. Gloves should be disposed of after use and if damaged.
Unless the person can remove their own medication from the packaging, it should be dispensed into a suitable container. For example, a medication pot.
This should be done without physically handling the medication wherever possible.
Check to make sure that the correct dose has been dispensed and prepared in line with the prescribers' instructions.
If the medicine is one that cannot come into contact with other medications the person is taking at that time, a second container will be needed.
Give the person their medication in line with the instructions in their individual care or support plan. This should include giving them their preferred drink etc.
Stay with the person whilst they take their medication.
Do not rush - allow the person time to take their medication at their own pace.
If the person is struggling to take oral medication in the form that it is currently in, seek consent to speak to their GP. Most solid medicines can be provided in liquid form.
Give medication to one person at a time - this avoids the risk of error.
All medicines administration records should:
- Be legible;
- Be signed by staff;
- Be clear and accurate;
- Have the correct date and time (either the exact time or the time of day the medicine was taken);
- Be completed as soon as possible after the person has taken the medicine;
- Avoid jargon and abbreviations.
A record must be made of all medication administered by, or in the service.
This includes:
- Medication taken by the person without support (self-medication);
- Medication administered by staff;
- Medication administered by visitors, including family members and health professionals.
The record must be made on a Medicines Administration Record (MAR) sheet.
The record must be checked and signed by 2 staff members.
If the person receives any kind of medication administration support, a record must be made each time that support is provided.
Sometimes, medication support will be shared between staff and an informal carer. If an informal carer has administered medication, this should also be recorded. The record can be made by the informal carer (if they have access to the record) or the staff member, whichever is agreed between the two.
The recording template should contain the following information and instructions for staff, in line with NICE recommendations:
- The name of the person and their date of birth;
- The name, formulation and strength of the medicine(s);
- How often or the time the medicine should be taken;
- How the medicine is taken or used (route of administration);
- The name of the person’s GP practice;
- Any stop or review date;
- Any additional information, such as specific instructions for giving medicine. For example, medicines to be taken with food (such as ibuprofen) or without food (such as some antibiotics).
The record made on the template should include:
- The name of the staff member/informal carer administering the medication;
- The name of the medication and dosage;
- The date and time administered;
- What support has been provided e.g., prompts, support to open a blister pack;
- Whether the medication was taken or refused.
The staff member/informal carer completing the record should sign it.
Note: If a person manages their medication with no support whatsoever, a record does not need to be made.
All medication records must be kept for 8 years after the person’s service has ended.
This includes records of:
- Ordering and supply;
- Administration;
- Medication errors, incidents or near misses;
- Disposal.
After 8 years, records should be reviewed and, if no longer needed, destroyed securely.
Covert administration is when medicines are given to someone without their knowledge or consent. This usually happens by crumbling the medicine into or hiding it within food.
If a person has the mental capacity to make decisions about medication, it is unlawful to give them medicines covertly. They have the right to refuse to take their medication, even if this is detrimental to their health and wellbeing.
However, the reason that they are refusing should be understood as it could be something easily rectified. For example, they may find a tablet difficult to swallow or not realise the benefit of taking it.
If a person lacks the capacity to make decisions about taking medication, giving it covertly does become an option to be explored. However, it should never be the first option.
It is only necessary and appropriate to give medication covertly when:
- The person actively and routinely refuses their medication; and
- They lack the capacity to make medication decisions; and
- A health professional or court has determined that taking the medication is in their best interests; and
- A health professional or court has decided that giving covert medication is the least restrictive way of administering the medication.
For further guidance see: Mental Capacity
The National Patient Safety Agency defines a medication error as
“A patient safety incident involving medicines in which there has been an error in the process of prescribing, dispensing, preparing, administering, monitoring, or providing medicine advice, regardless of whether any harm occurred”
Information about medication errors, including what to do if there is a medication error can be found in a separate chapter of this Handbook.
See: Information and Guidance for Specific Safeguarding Issues
All staff administering medication must have undertaken appropriate medication safety training. This should be refreshed regularly.
Some medication can only be provided by staff that have received specialist training and been deemed competent by a relevant health professional. This included epilepsy medication and non-oral routes of medication.
The registered manager should carry out quality assurance checks to make sure that medication is being administered safely, and that processes for ordering, transporting, storing, and disposing of medicines are also robust and being followed.
This process should involve checking MAR sheets, medicine stock levels, expiry of medication etc.
Last Updated: April 21, 2023
v30