Infection Prevention and Control (IPC)
Scope of this chapter
Infection: The invasion and multiplication of harmful pathogens, such as bacteria, viruses and parasites. Some pathogens have little effect at all (such as the common cold), but some can cause a more severe reaction or even death.
It is a legal requirement under Regulation 12 of the Health and Social Care Act 2008 to prevent and control infections. This should be done in line with The Code of Practice on the prevention and control of infections and related guidance:
Note: From time to time, the Department of Health and Social Care will issue additional or different guidance in response to new or current risks. It is the responsibility of the registered person and/or Designated Infection Prevention and Control Lead to keep abreast of such guidance and ensure it is implemented into infection prevention and control processes.
This chapter provides information about the different types of infection, how infection spreads and the infection prevention and control measures that we should all routinely take to manage risks. There is also a section of additional guidance for the registered person and/or the Designated Infection Prevention and Control Lead.
Relevant Regulations
Related Chapters and Guidance
- Ageing, Illness and Dying
- Assessing and Monitoring Health and Safety Risk
- Communicating Effectively
- Food Safety and Hygiene
- Infection Prevention and Control Inspections
- Risk Assessment (person-centred)
- Safe Care and Treatment
- Department of Health: Code of Practice on the prevention and control of infections and related guidance
- Department of Health and Social Care: Care homes - infection prevention and control
- CQC: Infection prevention and control in care homes
- CQC: Infection prevention and control in supported living services and extra care housing
- Skills for Care: Infection prevention and control
- NICE: Prevention infection quick guide
- CQC: Our infection prevention and control inspections
- Department of Health and Social Care: Linen processing within adult social care information sheet
- GOV.UK: Infection prevention and control in adult social care: acute respiratory infection
Amendment
In March 2024, a link to the GOV.UK guidance ‘Infection prevention and control in adult social care: acute respiratory infection’ was added to the ‘Related Chapters and Guidance’. This guidance contains measures to reduce the spread of viral acute infections, including COVID-19 in adult social care settings.
There are 3 different types of infection:
- Viral;
- Bacterial;
- Fungal.
Viral infections are caused by a virus. There are around 5,000 different known viruses that exist, although scientists believe there could be millions.
Viruses invade the person (host) and attach themselves to a cell. As they enter the cell, they release genetic material that forces the cell to replicate the virus and multiply.
Examples of viruses:
- Common cold;
- Coronavirus;
- Norovirus;
- Influenza (flu);
- Meningitis;
- Polio;
- Hepatitis C;
- HIV.
The immune system is designed to combat viruses and destroy the infected cells. The stronger the immune system the more effectively it will do this.
Vaccines do exist for some viruses. They cannot stop the virus from entering the body, but they can either prevent it from reproducing (either at all or less effectively) or boost the immune system to be able to better counter the effects of the virus.
Antibiotics are not effective against viruses.
Bacterial infections are caused by bacteria.
Not all bacteria are bad. For example, in our gut we have ‘good’ bacteria.
Examples of bacterial infections:
- Pneumonia;
- Gastritis;
- Food poisoning;
- Eye infections;
- Urinary tract infections (UTI);
- Skin infections;
- Sexually transmitted infections (STI).
Bacterial infections usually respond well to antibiotics.
A fungal infection is caused by a fungus.
Fungal infections normally affect the skin. They usually start in the upper layers and, if untreated, can progress to the deeper layers.
Sometimes fungal spores can be inhaled (such as yeast or mould). This can lead to infections such as Pneumonia.
Examples of fungal infections:
- Athletes foot;
- Ringworm;
- Fungal nail infection;
- Jock itch.
Infections can be spread from person to person in different ways:
- Skin contact;
- The transfer of bodily fluids;
- Contact with faeces;
- Ingesting contaminated food or water;
- Inhaling airborne particles or droplets;
- Touching an object that a person carrying the pathogen has also touched.
The speed at which an infection can spread will vary. Some infections can spread very quickly, such as the Norovirus or Coronavirus.
The following video shows just how easily and quickly infections can spread:
The infection prevention and control measures that we should all take are:
- Handwashing;
- Personal hygiene measures;
- Use the correct personal protective equipment (PPE);
- Clean the environment;
- Good food safety and hygiene;
- Dispose of waste safely;
- Handle sharps safely;
- Prevention through vaccination;
- Educate others.
Each of these measures is further explained below.
Note: If there is an infection present and therefore a risk of it spreading, additional measures may be implemented by the registered person. These will be in line with the latest government guidance and must be followed by all staff.
The registered person and/or the Designated Infection Prevention and Control Lead is responsible for ensuring that all the above measures are understood by staff, and that staff are provided with the resources they need to implement them. For example, enough PPE and cleaning supplies.
All staff members are responsible for making sure they understand the information provided to them, carry it out as instructed and report any barriers to doing so to the registered person and/or the Designated Infection Prevention and Control Lead.
Effective handwashing is an essential part of infection prevention and control.
Hands must always be washed:
- Before touching or handling any food;
- After touching raw meat, poultry, fish, eggs, unwashed vegetables and any packaging used for raw foods;
- After taking a break or going to the toilet;
- After touching or emptying bins;
- After any cleaning;
- After touching a cut or changing a dressing;
- After touching items touched or handled by others, such as phones, light switches, door handles or money;
- After touching your hair, face, blowing your nose, sneezing or coughing;
- Before helping residents with their meals/drink;
- After helping residents to use the toilet, bathe etc.;
- After emptying bed pans or commodes;
- After using medical equipment;
- Before and after handling medication;
- After touching dirty linen and clothing;
- After handling animals or their feeding bowls.
If someone already has an infection, hands must also be washed straight after touching objects that they have touched (e.g., chair, door handle, mug)
To wash hands effectively, see below.
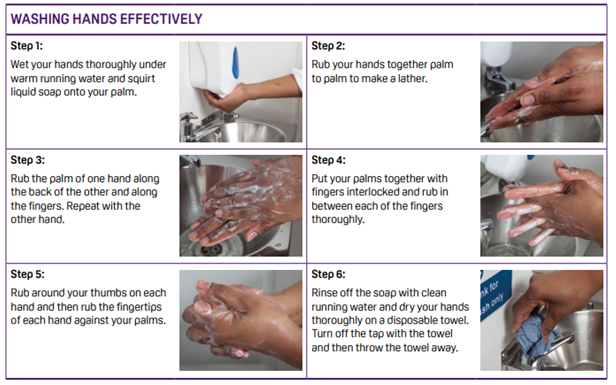
Source: Food Standards Agency
If you think another member of staff has not washed their hands, emphasise how important it is to do so. If they do not wash them straight away tell a manager or the registered person.
The following personal hygiene measures will reduce the risk of infection spreading and make it easier to wash hands effectively:
- Keep your arms bare below the elbow;
- Remove wrist and hand jewellery before starting work;
- Keep fingernails short and clean without nail polish or false nails;
- Cover any cuts or grazes with a waterproof plaster.
PPE includes disposable gloves, aprons and facemasks.
In a care home, use the right PPE for the task at hand.
In other settings, use PPE if it has been deemed necessary. Remember, in this case it must be made available for you to use.
- Only wear each item once;
- If gloves are being used, only put them on just before providing care and take them off again straight afterwards;
- Change gloves between care tasks for different people;
- Change gloves between different care tasks for the same person. For example, after helping with the toilet change before helping with a shower;
- Dispose of all PPE safely (see below).
Effective cleaning is essential to get rid of harmful bacteria and viruses.
Care homes
Cleaning should be carried out in line with the cleaning schedule/rota.
All cleaning and disinfection needs to be carried out in two stages:
- Clean: Using either hot, soapy water or a cleaning product (such as a sanitiser), remove visible dirt, grease and debris from surfaces/ equipment and wipe off or rinse;
- Disinfect: Following the manufacturer’s instructions, apply a disinfectant (such as a sanitiser) all over the surfaces/equipment and leave on for the required contact time.
It is important to complete this process in the correct order as chemical disinfectants only work if surfaces have been thoroughly cleaned first to remove grease and other dirt.
Remember, as well as cleaning surfaces and equipment, it is also important to clean other items that are touched regularly, such as light switches, telephones and door handles.
Other settings
Staff should make sure that all areas they use when providing support are clean before and after use. For example, food preparation areas and the toilet.
Remember, as well as cleaning surfaces and equipment, it is also important to clean other items that are touched regularly, such as light switches, telephones and door handles.
If infection is already present, cleaning supplies may need to be provided by the service to ensure that a two stage clean (as above) can take place.
If the care and support provided does not involve cleaning of the home, staff should educate the person about the benefits of cleaning and how to follow good cleaning infection control measures.
Maintaining a good standard of food safety and hygiene will reduce the risk of food related illness and infection.
There is a chapter of this Handbook dedicated to food safety and hygiene:
Waste that can spread infection must be disposed of safely.
For example:
- Used PPE;
- Dressings e.g., plasters;
- Continence pads.
In a care home there should be a designated hazardous/health waste facility.
In other settings or if this facility is not available, place the item into a sealed clinical waste bag.
The local authority can provide clinical waste bags and collect clinical waste from a care home or other residence. If you need to arrange this service, you can search ‘clinical waste collections’ in your area for information.
Note: Disposal of sharps requires specific measures to be safe. See below.
The government has produced an information sheet to support staff to take appropriate steps to reduce the risk of infection from contaminated linen.
This information sheet explains that for all linen in all settings ensure you:
- Always keep clean and used linen separate;
- Sore clean linen above floor level, in a clean, cool, dry place;
- Maintain stock rotation of linen, with the oldest linen used first.
To read the information sheet see Linen processing within adult social care: information sheet.
Sharps should only be used by staff that have received the relevant training and been deemed competent to do so.
- Handle sharps as little as possible and don't pass them from hand to hand;
- Do not bend, break or recap a used needle;
- Put used sharps in the right container straight away;
- Don't use sharps containers for anything else;
- Dispose of sharps containers when the fill line is reached, or every 3 months - whichever occurs first.
The local pharmacy or GP will be able to provide a sharps container/box. This can then be collected safely with other clinical waste.
Vaccinations can be an effective way to reduce the effect of a viral infection should it occur. For example, the Flu or Coronavirus vaccine.
Staff should seriously consider the benefits of vaccination when it is offered to them, including seeking advice from colleagues that may have already been vaccinated.
People being supported and their family and friends can play an important part in infection prevention.
Support and encourage them to understand why hand washing is important, when to wash their hands and how to do so effectively.
Staff working in someone’s home should also explain what they are doing to prevent infection, and how the person or family can support them. For example, not letting handsoap run out.
If a person becomes infected with any type of infection, the registered person and/or Designated Infection Prevention and Control Lead must be notified as soon as possible so that necessary additional infection control measures can be quickly implemented.
Staff must follow all guidance or additional measures implemented.
If staff have an infection, they should not come into work until the risks to others have been properly assessed. If risks cannot be managed safely, they should not return to work until a medical professional has deemed it safe for them to do so.
The service must have a Designated Infection and Prevention Control Lead. This can be the registered person but can be a separate appointment.
Note: The registered person remains legally responsible for any breaches of Regulation 12.
The service must have in place a full range of measures to manage and monitor the prevention and control of infection.
This includes:
- Risk assessments (see below);
- Systems for making sure staff are aware of their responsibilities and competent to meet them;
- Systems for identifying and reporting infections;
- Systems for communicating information about infections to staff, people using the service and any visitors, including immediate action to manage risk;
- Systems for how an infection or outbreak would be safely managed.
Guidance for setting up these systems and processes can be found in:
Department of Health: Code of Practice on the prevention and control of infections
The risks that must be assessed fall broadly into 3 categories:
- Generic risks;
- Risks that only affect certain staff members;
- Person-specific or activity-specific risks.
See: Assessing and Monitoring Health and Safety Risk
Risk assessments should be reviewed and updated periodically and whenever the need arises.
If staff have an infection and the risk to others cannot be safely managed, they should not come into work. They should not return to work until a medical professional has deemed it safe for them to do so.
Care homes
In a care home, the registered manager and/or Designated Infection Prevention and Control Lead must ensure that there are sufficient supplies to enable staff to meet their requirements around infection prevention and control. This includes PPE and cleaning supplies.
Non care home settings
If a risk assessment has deemed PPE necessary, the same rules apply as for care home settings.
Exceptional circumstances
If the situation is exceptional, for example there is a national pandemic, the local authority or NHS may be able to support with the provision of supplies over and above that which would normally be required.
The registered manager and/or Designated Infection Prevention and Control Lead must ensure that staff understand their responsibilities around infection prevention and control and are competent to meet those responsibilities.
All new starters should receive training as part of their induction, and this should be refreshed regularly.
Whenever new national guidance about infection prevention and control measures is implemented, changes and additional measures must be quickly and effectively communicated to staff.
An outbreak of an infection is classified as two or more people being infected.
As part of meeting Regulation 12, the service should already have systems in place for responding to an outbreak. This should include measures to reduce the risk of further spread, and how to communicate additional measures to staff, people using the service and visitors.
Local health protection team
The local health protection team must be notified of any outbreaks of infection. They may decide to take additional action to manage the health risk.
See: Find your local health protection team in England
CQC notification
Outbreaks of infection are not notifiable to CQC, unless:
- A person using the service has died;
- A person using the service has been seriously injured;
- There is a high level of staff absence;
- The outbreak has stopped the service running smoothly and safely.
See: Notifications
Notifying commissioners
The commissioning organisation should be notified whenever a CQC notification is made, a local health protection team notification is made and in any other circumstances set out in the contract between the service and the commissioning organisation.
If the service is at fault
If the reason that the infection outbreak has occurred is because good infection prevention and control measures were not followed, a safeguarding concern should be raised to the local authority.
See: Disclosure and Raising a Concern
If serious physical or psychological harm has occurred, the duty of candour may apply.
For further guidance see: Duty of Candour.
The registered person and/or Designated Infection Prevention and Control Lead must produce an annual statement to the CQC.
The annual statement should include:
- Information on incidents and outbreaks of infection;
- How the incident, or outbreak, was communicated to the person, staff and visitors;
- Infection prevention and control monitoring activity;
- Risk assessments that are in place;
- Training and competency assessments of staff around infection control;
- Review and update of policies, procedures and guidance;
- The actions that have been taken to rectify any complaints or incidents, in relation to infection prevention and control.
Last Updated: February 22, 2024
v40